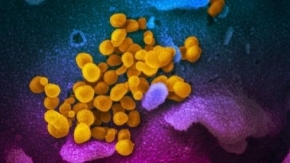
 In this ongoing series about impacts of the global COVID-19 pandemic, ECM explores innovations in research and advances in the innovation community toward finding treatments, vaccines, and a test for antibodies.
In this ongoing series about impacts of the global COVID-19 pandemic, ECM explores innovations in research and advances in the innovation community toward finding treatments, vaccines, and a test for antibodies.
By Helen Horvath
July 30, 2020 (San Diego’s East County) -- We all probably know of someone who has had COVID-19. This virus hit home earlier this month, when my 30-year-old nephew was diagnosed with COVID-19 after working as a contractor in Bakersfield at an Amazon facility, where employees reportedly had COVID-19. Contrary to the typical media images of people ill with COVID-19 who are hospitalized and on ventilators, my nephew was one of the approximately 75% of people who have been able to manage their coronavirus symptoms at home through doctor’s guidance and a 14-day quarantine. Everyone in my nephew’s home is now quarantined.
Even with precautions of masks and social distancing at work and in other public locations, the potential to contract and be exposed to COVID-19 is real. Families across the world are in need of treatments or a vaccine to save lives, as well as reliable antibodies testing to learn who may already have some limited immunities. In this article, we explore research protocols and share some advances toward attaining those important goals.
Over the past 20 years, research and how we develop solutions to national and global medical issues has changed substantially. When my sister worked as Director of Compliance at Johnson & Johnson 20 years ago, it could take up to 10 years to bring a medication to market. Yet, with advances in how the pharmacology industry obtains research dollars along with changes in how research is accomplished through rapid designing of prototypes, our government and non-government partners are now able to innovate solutions faster and wiser. This will prepare our nation for the next round of whatever illness may grow next.
COVID-19 is not just limited to humans. The virus has actually jumped from people to animals, as demonstrated at the Bronx Zoo. On April 22, 2020, the zoo announced that the big cats became ill when potentially infected by an asymptomatic employee who transmitted the COVID-19 to the big cats. This was determined through contact tracing – where the direct contact activities of the employee are tracked to determine who the person came in contact with. At the Bronx Zoo, additional animals have tested positive for SARS-CoV-2, the virus that actually causes COVID-19.
Globally other animals have also contracted COVID-19 including some pets believed to have contracted the disease from owners who were ill; yet, it is unknown whether wild and domestic cats or dogs can transmit SARS-CoV-2/COVID-19 to humans. More research needs to be done.
Meanwhile, through federal contracts and grants along with private partnerships, there are about 100 innovative vaccine programs underway between the various governments, drug makers, and researchers in the global community.
Our Tax Dollars at Work: Research Rules and Dollars
Many East County residents ask questions such as: “When will this be over?” “Do I really need a mask?” “When will we have a vaccine so that we can get back to normal?” We keep hearing “soon, soon, one year, two years, then soon again.” Yet what is the reality as our tax dollars are put to work?
Within the research arena, the United States federal government is the largest funder of research in our nation and often collaborates with other countries and organizations to create healthcare solutions. Each federal agency, Defense Department, military service, and the National Institute of Health has a massive budget for research and development. According to the Office of Management and Budget and the White House, in 2019 the President authorized $118.1Billion for federal research in areas such as agriculture, defense, commerce, education, and veterans affairs. This comprises approximately 92% of all public research and development (R&D) funding and does not include the specialized R&D tax credits to corporations involved in research.
Each agency’s specialized mission defines the type of R&D funding that is provided to the private sector partners. The three largest federal agencies that provide R&D funding are the Department of Defense, National Institute of Health, and Department of Energy. California firms and Universities have consistently received at least 20% of the federal R&D Budget since 2017. Additional R&D funds are distributed to Federal agencies to conduct internal research – such as the VA in San Diego.
According to clinicaltrials.gov, a government research registry and the World Health Organization (WHO), there are 23 vaccines in human clinical trials against the virus, SARS-CoV-2 or COVID-19 internationally. Additionally there are 23 COVID-19 specific research projects within the WHO’s research site. Additional research can be found on various segments of the research programs in the WHO database. The first firm that actually creates the first vaccine will most likely be the most financially successful in this pandemic environment.
In multiple articles relating to COVID-19, Dr. Anthony Fauci. The nation’s top infectious disease expert, has stated multiple times that the “hallmark of a vaccine is one that can actually mimic (the) natural infection and induce the type of response that you would get with natural infection…” In plain English, the vaccine must produce the same effects without causing the COVID-19 illness for the vaccine to be a success.
It takes six to ten months to have the Food and Drug Administration’s (FDA) approve the research plans and research for new drugs and therapies, once the initial data is gathered through a scientific research process. Although many vaccines and drugs are funded by the United States government, each firm must meet the standards set in the grant or contract for testing and evaluation. Yet, the reality is that the government agency paying for the research can obtain faster approval during national health emergencies such as COVID-19 or send the research back to the firm for more data or research. During the research process the life sciences firm will develop the product, determine dosage during the research phase and ensure that all federal research guidelines are followed.
Innovations in Treatment that are Questionable or Costly
Currently, no approved effective oral therapy or vaccine exists for the prevention of COVID-19 or for outpatient or inpatient treatment methods. As noted in ECM’s previous article about BIOCOM, the life sciences industry is learning as research continues, since the COVID-19 is a new strain of the Severe Acute Respiratory Syndrome (SARS) and related to the Middle Eastern Respiratory Syndrome (MERS).
Early on in the pandemic, hydroxychloroquine or chloroquine has been recommended as a potential treatment for outpatient COVID-19 care. These drugs are typically used to treat malaria and parasitic infections of the intestines. The studies into the effectiveness of this drug lacked proper research protocol for approval early in the pandemic. We have heard the President say to use this drug and state that he actually took the drug. Yet, what about the effectiveness and side effects of this drug or any drug or therapy?
Initially the FDA provided an emergency use authorization for the use of these chloroquine or hydroxychloroquine drugs for treatment of COVID-19 patients. The patients who received the drugs were in hospitals where clinical trials were not available. On June 15, 2020, the FDA revoked the emergency use authorization for use of this drug for the coronavirus. On July 1, 2020 the FDA published a summary of the safety issues pertaining to the use of hydroxychloroquine or chloroquine in COVID-19 patients. The FDA concluded a thorough investigation and reported that serious heart rhythm problems, blood and lymph system disorders, kidney injury, and liver problems and failure may happen as a result of the drug’s usage.
STATNews, an independent online professional digital news site for the biotech industry, reported on the overuse of ventilators for COVID-19. The report discusses the low blood oxygen levels of COVID-19 patients. These patients are not gasping for air, nor do they have a racing heart, or brains shutting down from lack of oxygen, typical triggers for use of ventilators.
According to the STATNews life sciences article, these factors have caused a reassessment of medical protocols for treatment of COVID-19 patients in hospitals, especially as intensive care units (ICU) reassess how fast a patient is put on a ventilator based upon their blood oxygen levels. The medical industry is currently evaluating the effectiveness of using mechanical ventilators immediately upon hospitalization.
The ventilator treatment has a side effect; the patient’s air sacs in the lungs begin to fill with a gummy yellow fluid that limits the ability to transfer oxygen from the blood to the lungs, creating greater health decline in COVID-19 patients on ventilators. This creates a need to force higher air flow that may damage the lungs and pulmonary system. Air does not transfer to the blood with oxygen due to the yellow gummy substance for those with Acute Respiratory Distress Syndrome (ARDS). This information was confirmed in a letter to the American Journal of Respiratory and Critical Care Medicine by German and Italian researchers. The researchers stated that COVID-19 was unlike “any other…acute respiratory distress”. The authors of the letter stated that doctors “need to use the gentlest possible ventilation to reduce damage to the lungs and pulmonary system.” Basically, old theories of treatment in the beginning of the pandemic may not be as effective as newer treatment methods that are evolving daily.
 The use of Extracorporeal Membrane Oxygenation (ECMO) is similar to a heart and lung bypass machine that is used in open heart surgery.
The use of Extracorporeal Membrane Oxygenation (ECMO) is similar to a heart and lung bypass machine that is used in open heart surgery.
The ECMO machine can be used simultaneously for heart and lung problems or only lung problems to clean the blood of patients with ARDS or COVID-19. The University of San Francisco and other medical centers have the ECMO for patients who are recovering from heart or lung failure among other uses. The risk of using the ECMO includes infection, transfusion issues, air bubbles in the tubing, and increased chance of stroke. This procedure may not be for everyone due to the high cost of using the machine and also the risk of dying anyway. Also, ECMO machines may not be available in more rural regions.
Yet, the World Health Organization’s interim guidelines for treatment of COVID-19 as outlined in the Lancet on May 1, 2020, includes recommendations for the use of ECMO machines to treat COVID-19 as a potential treatment as new therapies are developed.
The ECMO is generally tied to those with acute respiratory distress syndrome (ARDS). ARDS is a more serious active symptom of COVID-19 and may appear as pneumonia. Dr. Chethan Sathya, a pediatric surgeon and journalist based in New York City, stated in a Washington Post article that “the use of the ECMO is a last ditch “Hail Mary” option to keep a patient alive.“ In the surgical procedure to connect the ECMO, there are risks as outlined by Dr. Sathya when inserting a large tube in two major arteries. The ECMO acts as a “blood cleaner” by adding missing oxygen to the blood as it is processed through the machine creating bright red blood versus the dark red blood lacking oxygen.
According to Dr. Chethan, the initial research results from Wuhan, China showed that 11.5% of COVID-19 patients required the use of an ECMO machine. Yet the sad part was that out of six patients only one COVID-19 patient survived with ECMO. ECMO is very labor intensive on the part of the healthcare workers and very costly to the patient. Across the United States, ECMO was used successfully on a patient in Chicago who survived.
Yet, data in the United States on the usage of ECMO is limited based upon 1201 ECMO cases in North America. Of these numbers 215 patients are still on ECMO with 868 discharged dead or alive. Across the globe only 744 people out of 1245 people with COVID-19 were discharged alive with ECMO treatment. Although effective for some, again, the risks of further organ damage due to the ARDS disease progression may not be a viable therapy for everyone with COVID-19.
Current Research: Innovations in the Works – including advances in San Diego
Initially, the SARS-CoV-2/COVID-19 virus was slippery like a fish when caught. Scientists did not have a great handle on how the virus entered the body, how it becomes a virus, and solutions for prevention and cures for COVID-19. Yet times are changing in labs across the country as the global community searches for solutions to this often deadly virus. Finding a therapy for COVID-19 that will prevent the virus and also treat the virus has been particularly challenging.
 Some of the most promising research has grown in our own backyards. The University of California San Diego (UCSD) has completed a unique technology research project which created a hypothesis that certain currently available drugs classified as protease inhibitors would not permit the virus to bind with angiotensin converting enzyme inhibitor (ACE2). Without intervention, ACE2 receptors allow the virus that causes COVID-19 to infect and destroy our cells.
Some of the most promising research has grown in our own backyards. The University of California San Diego (UCSD) has completed a unique technology research project which created a hypothesis that certain currently available drugs classified as protease inhibitors would not permit the virus to bind with angiotensin converting enzyme inhibitor (ACE2). Without intervention, ACE2 receptors allow the virus that causes COVID-19 to infect and destroy our cells.
The process is similar to putting on a pair of snug jeans; then attempting to zip your jeans. Zipper does not close, the pants will not fit. With COVID-19 the ACE2 receptor permits the COVID-19 in the front door. The protease inhibitors keep the front door locked when the drug is taken. Yet, not all FDA approved protease inhibitor drugs will work to prevent COVID-19.
The UCSD research was designed and executed using the San Diego Supercomputer Center through computer modeling and artificial intelligence. The researchers simulated how the COVID-19 virus would interact with the drug. Basically, the simulated virus would “dock” into the drug to predict how the drug would fit into a particular spot on the virus. Similar to parking a care into a stall, the drug must fit in the parking spot to stop the virus from multiplying in the body.
The researchers examined the list of FDA-approved protease inhibitors to determine if the drugs would potentially stop COVID-19. Using technology, UCSD selected 64 potential COVID-19 protease inhibitors to test at the University. Through technology, the UCSD study found 64 potential protease inhibitor FDA approved drugs that may work to prevent COVID-19. Through scientific data mining, the researchers were able to determine the potential effectiveness of these protease inhibitors to block COVID-19; yet, more needs to be accomplished before announcing full success.
Scientists research the effectiveness in the hunt for a COVID-19 treatment. Many researchers have turned towards HIV drugs to determine effectiveness of a medication. The most promising drugs from a global study include 1)Tipranavir, 2) Indinavir 3) Atazanavir 4) Darunavir and 5) Ritonavir. Many of these drugs are protease inhibitors.
According to the New England Journal of Medicine dated May 22, 2020, 1059 test subjects were entered and completed the recent Remdesivir study under a National Institute of Health Allergy and Infectious Disease and ACTT-1 Clinical Trials.gov research grant. The study divided the 1059 participants into two groups: a placebo group of 521 people who did not get the treatment only fake medication and 538 who were assigned to take Remdesivir. The entire group of study participants had lower respiratory tract infections when hospitalized. According to the research results, Remdesivir showed some promise in adults hospitalized with COVID-19 and evidence of lower respiratory tract infection. Yet, more research is needed.
Additionally, the World Health Organization (WHO) reported that Dexamethasone, a corticosteroid that is used in a wide range of conditions for its anti-inflammatory and immunosuppressive effects, was tested recently in the United Kingdom. The United Kingdom’s national clinical trial RECOVERY that used Dexamethasone was found to have benefits for critically ill COVID-19 patents on ventilators. According to the World Health Organization, the use of this drug demonstrated a reduction in patient deaths of about 33% for those on ventilators. For patients requiring only oxygen, overall mortality was reduced by 1/5th. Yet again, more research needs to be accomplished with a greater pool of subjects.
It was announced that Inovio Pharmaceuticals was recently awarded a $71 million contract from the Department of Defense. The contract was awarded to scale up production of the firm’s next generation Cellectra device that will be used to administer the COVID-19 vaccine into the skin. The device is a small hand-held tool that is used to administer safe doses of medication to patients. Inovio has already begun human testing in April 2020 of its vaccine. As there are currently no vaccines for COVID-19 approved by the government. This research award is a first step towards finding a vaccine. Though other research groups may disagree. Inovio’s vaccine is purported to produce antibodies and immune system protective responses in guinea pigs and mice. It is anticipated that if Inovio’s efforts are successful, the future in 2021 will look bright with the expected release of hundreds of millions of doses of their vaccine.
Moderna, a biotech company, is one of many industry corporations developing a vaccine for COVID-19. The vaccine has been reported to supposedly generate immunity responses similar to people who have had the virus and then recovered. The vaccine is being developed in conjunction with the National Institute of Allergies and Infectious Diseases (NIAID) who has strict standards for research.
On or about May 18, 2020 Moderna released a public statement regarding the success of the COVID-19 vaccine named mRNA-1273. Under federal guidelines research organizations must have a “representative sample”. This was a premature announcement that caused Moderna's stock to increase almost immediately. The prematurity of the announcement and increase in stock price created an ethical dilemma since the vaccine trials are clearly tied to research standards and number of participants in the study.
Eight people does not meet the ethical guidelines for a representative sample required to call a research project phase I study a success.
Ethical standards in research are key to the community when reading social media posts or non-scientific media such as newspapers, magazines or blog posts. When reading about fantastic new therapies or vaccines, please read the research data as recommended by BIOCOM. Sometimes the government will overlook research standards for the “greater good”. This often does not bode well for vaccines or therapies when short cuts are taken. The industry, according to BIOCOM, questions the actual success and ability to deliver a COVID-19 vaccine that is effective.
Companies can get away with being a bad actor in crisis situations. Yet, industry associations and firms tend to police each other in the research and development field. Bad actors can divert focus to their product through misleading press releases that cause their stock to rise while not having sufficient data to warrant the success statements in the press. Through this the media distraction causes a slowdown in the actual development of appropriate therapies to create and cure diseases. This is why ethics is so important to the life sciences research and development process.
Safety in Research
In reading the announcement that UCSD will participate in the Moderna vaccine trials, there is concern over potential for people becoming ill as a result of Moderna not following research protocol in this rush to make “big bucks.” Someone at the National Institute of Health NIH)NIAID is supporting this firm. There is speculation in the stock market over who will make the first vaccine for COVID-19. Yet, what is actually within the proposed drugs, therapies, and vaccines that our community will be asked to take? Will you stand at the well, take a shot and hope for the best?
Human trials for an untested product with exceedingly small numbers of people in the test do not address the fact that there are not enough people currently tested. One of the issues with many of these prototypes is the delivery method within the body to administer and accept the vaccine. It is not about the needle in the arm; rather, the concern is what happens when the drug enters your body and begins interacting with your cells.
Moderna and UCSD are conducting a study of the mRNA-1273 vaccine. Sounds educated right? Cool title, butwhat does mRNA mean? The short version is mRNA or messenger ribonucleic acid or RNA. What many people may not understand is that this particular vaccine uses your own DNA code to process and synthesize mRNA. The mRNA is a single stranded RNA molecule that is tied to how your body’s genetic map or sequence is designed. Like your DNA, mRNA genetic information is a copy of a previous molecule. Mistakes in the molecule are copied along with other information in the molecule. The mRNA carries genetic coding to other parts of the cell to process through three phases. Once the molecule has reached the end of their lifecycle the molecule begins the process again. The information in the molecule typically does not change unless the information in the mRNA changes.
Pfizer Pharmaceutical and a German biotechnology firm, BioNTech, was recently contracted for 600 million doses of a vaccine. The firm’s 100 million doses are promised to the government before the end of 2020. Pfizer and BioNTech will include 30,000 people from Brazil, Argentina, Germany, and 39 states in the United States.
Just as with Moderna’s vaccine, the Pfizer/BioNTech uses mRNA to teach the body what SARS-COV-2 looks like by changing the genetic information so that when exposed to SARS-COV-2, the body may recognize and attack the virus. Both vaccines are designed to change the genetic reaction to COVID-19.
The irony is that in the COVID-19 research environment,often the rules seem not to apply to some and may not ensure the drug causes no serious harm due to the ‘fast track’ or political “warp speed” research rules to permit quicker drugs and therapies to market. The irony is that UCSD Health will begin to offer Moderna’s mRNA-1273 vaccine during trials to 500 people and eventually up to 30,000 people.
The questions to consider when volunteering for a study or taking a new medicine include what the product is made of and how it will interact with your body. Ask yourself under what circumstances will you participate in this research? Most importantly, did you research thoroughly the firm who developed the vaccine and how they conducted their research? Was it ethical, or was there a potential questionable rush to market? Remember the term “representative sample” as you move forward through potentially volunteering for this study. Be open to new therapies while at the same time being cautious of the actual therapy if the research did not follow protocol. To learn about the drug, consider a source such as the New England Journal of Medicine to determine the research. Since NIH is funding the research; you may find skewed statements in their announcements of a particular trial.
Antibodies advances
Another field of research involves finding an accurate test to assess whether people have developed antibodies after recovering from COVID-19 or perhaps being an asymptomatic carrier. While no one knows how long antibodies may offer protection from the virus, the race to develop an accurate antibodies test appears to have had a major breakthrough locally with San Diego based Truvian Sciences.
Some early antibody tests used in the U.S. were notoriously unreliable, with 40% inaccuracy rates, and problems with how research was conducted. BioSpacereported on July 29, 2020 that the U.S. Food and Drug Administration (FDA) announced emergency use approval to Truvian Sciences of a COVID-19 antibodies known as Easy Check COVID-19 IgM/IgG™ Test. The test was evaluated by test was evaluated and tested by University of California, University of Chicago, and Frederick National Laboratory for Cancer Research (FNLCR) prior to FDA approval. Currently Easy Check COVID-19 IgM/IgG™ Testrequires a full blood draw, but other news media reports indicated that Truvian is working on a finger-prick version.
International pandemic moved our nation further towards global unity in research
 The scientific community understands the initial origins of COVID-19 in Wuhan, China. Yet, months later, world leaders gathered on March 26, 2020, at a Global (G20) Summit to address the COVID-19 crisis. The G20 Summit became “a powerful reminder of the interconnectedness and vulnerabilities” of vulnerable populations in our global communities. As you may remember, people who traveled from overseas to the United States carried the COVID-19 virus and people from areas of the United States to overseas also carried the virus, infecting global communities.
The scientific community understands the initial origins of COVID-19 in Wuhan, China. Yet, months later, world leaders gathered on March 26, 2020, at a Global (G20) Summit to address the COVID-19 crisis. The G20 Summit became “a powerful reminder of the interconnectedness and vulnerabilities” of vulnerable populations in our global communities. As you may remember, people who traveled from overseas to the United States carried the COVID-19 virus and people from areas of the United States to overseas also carried the virus, infecting global communities.
At the end of the G20 Summit, global leaders stated that they would do “whatever it takes to overcome the pandemic.” The participants of the G20 summit agreed to interject $5 trillion into the global economy to slow or cut back the social and economic impacts of the pandemic on our global communities. Yet what can we learn as a community and nation as the global community works to collaborate to find immunizations and cures for the SARS-CoV-2/COVID-19 virus?
The National Institute of Allergies and Infectious Diseases (NIAID), a branch of the National Institute of Health, has created a Fiscal Year 2020-2024 strategic plan for COVID-19 research in our nation. The larger NIH has an organizational strategic plan for COVID-19 Research. This plan includes the five strategic priorities guide that includes plans for innovation and solutions to stop COVID-19. Within the research guidelines are the rapid response research options, many of which are centered in San Diego, along with universities, labs, and biotechnology and biopharmaceutical firms across the nation and globally.
On April 29, 2020, NIH announced a new initiative that will speed innovation, development and commercialization of COVID-19 testing technology through the Rapid Acceleration of Diagnostics (RADx) to infuse federal funding for small and large firms researching solutions to COVID-19 testing and immunization. The NIH has also launched public-private partnerships to speed upon the development and treatment options for COVID-19. This effort includes more than a dozen biopharmaceutical firms that will perform both development of a vaccine and testing through clinical trials. By leveraging these government and non-government assets the local, state, and federal government will have the capability to develop current and future responses to pandemics nationally and in cooperation with other countries.
Contact tracing is currently used in the COVID-19 environment by health departments to identify and track the movement of infectious diseases. Through contact tracing, researchers are able to identify people who have an infectious disease (cases) and their contacts (people who may have been exposed to COVID-19) and work with these individuals to interrupt disease transmission. This is part of the reason the San Diego Health Department and State of California have asked exposed residents to voluntarily self-isolate and to quarantine at home. Contact tracing allows researchers to gather more accurate data from a broader region.
For research, contact tracing for COVID-19 typically involves:
- Interviewing people with COVID-19 to identify everyone with whom they had close contact during the time they may have been infectious
- Notifying contacts of their potential exposure,
- Referring contacts for testing,
- Monitoring contacts for signs and symptoms of COVID-19 and
- Connecting contacts with services they might need during the self-quarantine period.
In addition, contact tracing allows those who recovered from COVID-19 to participate in anti-body and other studies designed for those who potentially have resistant COVID-19 cells. An example of this includes Moderna Biotech firm’s mRNA-1273 potential vaccine.
Part of research and innovation is to create cycles of rapid innovation. Yet some of the innovations have the potential to create death in the COVID-19 recovery cycle from pre-existing conditions, mistakes made during surgeries or research, or other demographic information. When dealing with therapies and research, it is better to fail early and often during innovative research. This allows the research community to learn faster, collaborate better, and modify attempts to create vaccines and therapies that will actually work with appropriate research testing and development. This will take strict research protocols and more than eight people in a study to create the needed solutions. Unfortunately, this also will take time, something that residents are running out of as COVID-19 continues to spread, increasing the health and economic tolls on communities.
For more information about the current COVID-19 data, please go to the Center for Disease Control or NIH’s NIAID website for latest research in COVID-19.
 Dr. Helen Horvath is a psychologist, organizational development consultant and published author on a variety of psychology and business topics. As a speaker, she has presented at the American Psychological Association Annual Conference, Society of Industrial and Organizational Psychology, and other key professional organizations. She is a former marriage and family therapist and published a relationship book entitled “Put a Period to IT: When Divorce is the Option”. Dr. Horvath writes for East County Magazine on COVID-19 topics in business, healthcare, and research as part of the Facebook Grant Project.
Dr. Helen Horvath is a psychologist, organizational development consultant and published author on a variety of psychology and business topics. As a speaker, she has presented at the American Psychological Association Annual Conference, Society of Industrial and Organizational Psychology, and other key professional organizations. She is a former marriage and family therapist and published a relationship book entitled “Put a Period to IT: When Divorce is the Option”. Dr. Horvath writes for East County Magazine on COVID-19 topics in business, healthcare, and research as part of the Facebook Grant Project.
East County Magazine gratefully acknowledges the Facebook Journalism Project for its COVID-19 Relief Fund grant to support our local news reporting including impacts on vulnerable communities during the COVID-19 pandemic. Learn more: #FacebookJournalismProject and https://www.facebook.com/fbjournalismproject/.
You can donate to support our local journalism efforts during the pandemic at https://www.EastCountyMedia.org/donate.







Recent comments